Overview
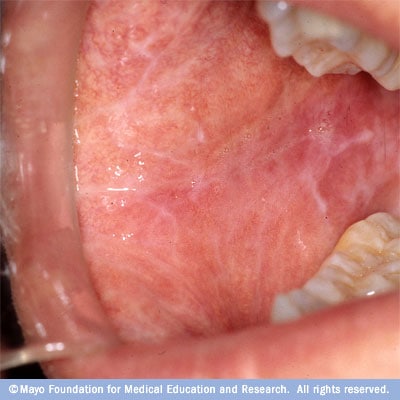
Oral lichen planus can't be passed from one person to another. The disorder occurs when the immune system mounts an attack against cells of the oral mucous membranes for unknown reasons (autoimmune disorder).Oral lichen planus (LIE-kun PLAY-nus) is an ongoing (chronic) inflammatory condition that affects mucous membranes inside your mouth. Oral lichen planus may appear as white, lacy patches; red, swollen tissues; or open sores. These lesions may cause burning, pain or other discomfort.
Symptoms can usually be managed, but people who have oral lichen planus need regular monitoring because they may be at risk of developing mouth cancer in the affected areas.
Symptoms
Signs and symptoms of oral lichen planus affect the mucous membranes of the mouth.
Appearance
The lesions may appear as:
- Lacy, white, raised patches of tissues
- Red, swollen, tender patches of tissues
- Open sores
Location
These lesions may appear on the:
- Inside of the cheeks, the most common location
- Gums
- Tongue
- Inner tissues of the lips
- Palate
Pain or discomfort
The white, lacy patches may not cause discomfort when they appear on the inside of the cheeks. However, symptoms accompanying red, swollen patches and open sores may include:
- Burning sensation or pain
- Sensitivity to hot, acidic or spicy foods
- Bleeding and irritation with tooth brushing
- Inflammation of the gums (gingivitis)
- Painful, thickened patches on the tongue
- Discomfort when speaking, chewing or swallowing
Other types of lichen planus
If you have oral lichen planus, you may have lichen planus lesions affecting other parts of your body.
- Skin. Lesions usually appear as purplish, flat-topped bumps that are often itchy.
- Genitals. Lesions on the female genitalia often cause pain or burning and discomfort with intercourse. The lesions are usually red and eroded and occasionally appear as white areas. Lesions also can occur on male genitalia.
- Ears. Lichen planus of the ears can lead to hearing loss.
- Scalp. When skin lesions appear on the scalp — a rare condition — they may cause temporary or permanent hair loss.
- Nails. Though rare, lichen planus of the toenails or fingernails may result in ridges on the nails, thinning or splitting of nails, and temporary or permanent nail loss.
- Eyes. Rarely, lichen planus may involve the mucous membrane surfaces of the eyes, and can cause scarring and blindness.
- Esophagus. Lichen planus of the esophagus also is rare, but when it occurs, it may result in a narrowing of the esophagus or the formation of tightened, ringlike bands in the esophagus that can make swallowing difficult.
Causes
It's not known what causes oral lichen planus. However, T lymphocytes — certain white blood cells involved in inflammation — appear to be activated in oral lichen planus. Although it could indicate an immune disorder, more research is needed to determine the exact cause.
It's possible that, in some people, oral lichen planus may be triggered by certain medications, mouth injury, infection, or allergy-causing agents such as dental materials. However, these causes are not confirmed.
Risk factors
Some factors may increase your risk of developing oral lichen planus, such as having a disorder that compromises your immune system or taking certain medications, though more research is needed.
Complications
Severe cases of oral lichen planus may increase the risk of:
- Significant pain
- Weight loss or nutritional deficiency
- Stress or anxiety
- Depression
- Scarring from erosive lesions
- Secondary oral yeast or fungal infections
- Oral cancer
Diagnosis
Your doctor makes a diagnosis of oral lichen planus based on:
- Discussion of your medical and dental history and the medications you're taking
- Review of symptoms, including lesions in your mouth and any other places on your body
- Examination of your mouth, and other areas as appropriate
He or she also may request lab tests such as:
- Biopsy. A small tissue sample is taken from one or more lesions in your mouth and examined under a microscope to look for indications of oral lichen planus. Other more specialized microscopic tests may be needed to identify immune system proteins commonly associated with oral lichen planus.
- Cultures. A sample of cells is taken from your mouth using a cotton swab. The sample is examined under a microscope to determine whether you have a secondary fungal, bacterial or viral infection.
- Blood tests. These may be done to identify conditions such as hepatitis C, which may rarely be associated with oral lichen planus, and lupus, which may look similar to oral lichen planus.
Treatment
Oral lichen planus is a chronic condition. There is no cure, so the treatment focuses on helping severe lesions heal and reducing pain or other discomfort. Your doctor will monitor your condition to determine the appropriate treatment or stop treatment as necessary.
If you have no pain or discomfort and if only white, lacy lesions are present, you may not need any treatment. For more severe symptoms, you may need one or more of the options below.
Symptomatic treatment
Treatments such as topical numbing agents can be used to provide temporary relief for areas that are particularly painful.
Corticosteroids
Corticosteroids may reduce inflammation related to oral lichen planus. One of these forms may be recommended:
- Topical. Mouthwash, ointment or gel is applied directly to the mucous membrane — the preferred method.
- Oral. Corticosteroids are taken as a pill for a limited amount of time.
- Injection. The medication is injected directly into the lesion.
Side effects vary, depending on the method of use. Talk with your doctor to weigh the potential benefits against possible side effects.
Immune response medicines
Medications that suppress or modify your body's immune response may be used to improve more-severe lesions and lessen pain. They come in these forms:
- Topical ointments or gels. Calcineurin inhibitors, similar to oral drugs used to prevent rejection of transplanted organs, may be effective for treating oral lichen planus. But these medications have a Food and Drug Administration warning because of an unclear association with cancer. Examples include tacrolimus (Protopic) and pimecrolimus (Elidel).
- Systemic medication. For severe cases where oral lichen planus also involves other areas — such as the scalp, genitalia or esophagus — systemic medications that suppress the immune system may be used.
Dealing with triggers
If your doctor suspects that oral lichen planus may be related to a trigger, such as a drug, an allergen or stress, he or she can recommend how to address the trigger. For example, you may be advised to try another drug instead, to see an allergist or dermatologist for additional testing, or to learn stress management techniques.
Lifestyle and home remedies
In addition to regular medical and dental treatment, self-care measures may help improve your oral lichen planus symptoms or help prevent recurring episodes of severe symptoms:
- Practice good oral hygiene. Keep your mouth clean to reduce your symptoms and help prevent infection. Gently brush your teeth at least twice a day using a bland toothpaste, and floss daily.
- Adjust your diet. Cut out spicy, salty or acidic foods if they seem to trigger or worsen your symptoms. Choose foods that are soft to help limit discomfort. And reduce or eliminate the use of caffeine.
- Avoid irritants. Avoid alcohol or tobacco. Also avoid habits that can injure the inside of your mouth, such as chewing on your lip or cheek.
- Learn to manage stress. Because stress may complicate symptoms or trigger symptom recurrence, you may need to develop skills to avoid or manage stress. Your doctor may refer you to a mental health specialist who can help you identify stressors, develop stress management strategies or address other mental health concerns.
- See your doctor or dentist regularly. See your dentist twice a year for checkups and cleanings, or more often as directed by your dentist. Because long-term treatment is often required, talk to your doctor or dentist about how often you should be seen to evaluate how your treatment is working and for cancer screening.